Meningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs. Meningitis can be life-threatening because of the inflammation's proximity to the brain and spinal cord; therefore the condition is classified as a medical emergency.
The most common symptoms of meningitis are headache and neck stiffness associated with fever, confusion or altered consciousness, vomiting, and an inability to tolerate light (photophobia) or loud noises (phonophobia). Sometimes, especially in small children, only nonspecific symptoms may be present, such as irritability and drowsiness. If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash.
A lumbar puncture may be used to diagnose or exclude meningitis. This involves inserting a needle into the spinal canal to extract a sample of cerebrospinal fluid (CSF), the fluid that envelops the brain and spinal cord. The CSF is then examined in a medical laboratory. The usual treatment for meningitis is the prompt application of antibiotics and sometimes antiviral drugs. In some situations, corticosteroid drugs can also be used to prevent complications from overactive inflammation. Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalus and cognitive deficits, especially if not treated quickly. Some forms of meningitis (such as those associated with meningococci, Haemophilus influenzae type B, pneumococci or mumps virus infections) may be prevented by immunization.
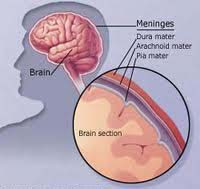
Meningitis is an infection of the meninges. The meninges are the three layers of membranes surrounding the brain and spinal cord. The outermost layer of the meninges is the dura mater, the central layer is the arachnoid, and the layer closest to the brain is the pia mater. In between these layers is a liquid called cere-brospinal fluid that protects the brain.
Infections reach the meninges by entering the cerebrospinal fluid. At this point, the meninges become irritated and swollen. This swelling is what produces the classic meningitis symptoms of stiff neck and headache. Bacterial meningitis is common in the United States; at least 25,000 cases are diagnosed each year.
In adults, a severe headache is the most common symptom of meningitis – occurring in almost 90% of cases of bacterial meningitis, followed by nuchal rigidity (inability to flex the neck forward passively due to increased neck muscle tone and stiffness). The classic triad of diagnostic signs consists of nuchal rigidity, sudden high fever, and altered mental status; however, all three features are present in only 44–46% of all cases of bacterial meningitis. If none of the three signs is present, meningitis is extremely unlikely. Other signs commonly associated with meningitis include photophobia (intolerance to bright light) and phonophobia (intolerance to loud noises). Small children often do not exhibit the aforementioned symptoms, and may only be irritable and look unwell. In infants up to 6 months of age, bulging of the fontanelle (the soft spot on top of a baby's head) may be present. Other features that might distinguish meningitis from less severe illnesses in young children are leg pain, cold extremities, and an abnormal skin color.
Nuchal rigidity occurs in 70% of adult cases of bacterial meningitis. Other signs of meningism include the presence of positive Kernig's sign or Brudzinski's sign. Kernig's sign is assessed with the patient lying supine, with the hip and knee flexed to 90 degrees. In a patient with a positive Kernig's sign, pain limits passive extension of the knee. A positive Brudzinski's sign occurs when flexion of the neck causes involuntary flexion of the knee and hip. Although Kernig's and Brudzinski's signs are both commonly used to screen for meningitis, the sensitivity of these tests is limited. They do, however, have very good specificity for meningitis: the signs rarely occur in other diseases. Another test, known as the "jolt accentuation maneuver" helps determine whether meningitis is present in patients reporting fever and headache. The patient is told to rapidly rotate his or her head horizontally; if this does not make the headache worse, meningitis is unlikely.
Meningitis caused by the bacterium Neisseria meningitidis (known as "meningococcal meningitis") can be differentiated from meningitis with other causes by a rapidly spreading petechial rash which may precede other symptoms. The rash consists of numerous small, irregular purple or red spots ("petechiae") on the trunk, lower extremities, mucous membranes, conjuctiva, and (occasionally) the palms of the hands or soles of the feet. The rash is typically non-blanching: the redness does not disappear when pressed with a finger or a glass tumbler. Although this rash is not necessarily present in meningococcal meningitis, it is relatively specific for the disease; it does, however, occasionally occur in meningitis due to other bacteria. Other clues as to the nature of the cause of meningitis may be the skin signs of hand, foot and mouth disease and genital herpes, both of which are associated with various forms of viral meningitis.
Meningitis is sometimes difficult to detect in infants and small children because its classic symptoms may be subtle or absent. A baby cannot tell you that he or she has a headache, so doctors must be very observant in order to properly diagnose what is wrong. A baby with meningitis may display irritability, lack of appetite, and/or vomiting. At any age, seizures may result as the disease progresses, followed by coma and death. Meningitis can originate from many different causes, including viral, fungal, bacterial, parasitic, cancerous, and chemical.
Meningitis is potentially life-threatening and has a high mortality rate if untreated; delay in treatment has been associated with a poorer outcome. Thus treatment with wide-spectrum antibiotics should not be delayed while confirmatory tests are being conducted. If meningococcal disease is suspected in primary care, guidelines recommend that benzylpenicillin be administered before transfer to hospital. Intravenous fluids should be administered if hypotension (low blood pressure) or shock are present. Given that meningitis can cause a number of early severe complications, regular medical review is recommended to identify these complications early, as well as admission to an intensive care unit if deemed necessary.
Mechanical ventilation may be needed if the level of consciousness is very low, or if there is evidence of respiratory failure. If there are signs of raised intracranial pressure, measures to monitor the pressure may be taken; this would allow the optimization of the cerebral perfusion pressure and various treatments to decrease the intracranial pressure with medication (e.g. mannitol). Seizures are treated with anticonvulsants. Hydrocephalus (obstructed flow of CSF) may require insertion of a temporary or long-term drainage device, such as a cerebral shunt.
Viral Meningitis
One of the most common, but least dangerous, torms of meningitis is viral meningitis. Viral meningitis will normally clear up by itself without complications. Viral meningitis is sometimes called aseptic meningitis when doctors attempt but fail to produce a positive identification of the underlying virus. Nearly every aseptic meningitis is caused by a virus.
Many different viruses can cause meningitis, including herpes simplex types 1 and 2, mumps, influenza, Epstein-Barr, measles, rubella, and polio, among others. The most common causes of viral meningitis are enteroviruses. These viruses normally live in the intestines. Enteroviruses like coxsackie and echovirus are often the cause of viral meningitis. Since many people who have it do not get sick enough to seek medical attention, it is difficult to know how widespread viral meningitis might be. Statistics are only available for the cases severe enough to require hospitalization.
In populations where vaccinations are common, some of these causes of meningitis are rare. In the United States, for instance, meningitis from the mumps would be extremely unusual. However, in unimmu-nized populations, a full 30 percent of the people who contract the mumps virus will develop viral meningitis. Strangely, males are two to five times more likely than meningitis in this way.
1991, for example, 636 cases of aseptic meningitis were reported to the New York State Department of Health. This represented a 153 percent increase over the average number of cases for this period. The viruses responsible for this outbreak were coxsackie and echoviruses.
Other viruses that may cause meningitis include those spread by mosquitoes and ticks, like the St. Louis encephalitis virus, the eastern equine encephalitis virus, and the Colorado tick fever virus.
Fungal Meningitis
Fungi can also cause meningitis. Candida, Histoplasma, Coccidioides, and Cryptococcus fungi have all been responsible for meningitis infections. Most cases of fungal meningitis occur in people who are alieady sick with a disease like AIDS, which has suppressed their immune systems. The fungi that cause meningitis are found in the environment and are spread on air currents. Healthy people will not develop meningitis from breathing in these particles. Several of these fungi are found in soil and others, like Candida, aie found everywhere, including on human skin and inside the intestines.










0 comments:
Post a Comment